#7 Kazuhiko Maekawa
Senior Adviser/ Director, the Izumi Health Service Facility for the Elderly, Meiwa Kai/ Professor Emeritus of Tokyo University/ Honorary Director of Kanto Central Hospital of the Mutual Aid Association of Public School Teachers
The 7th iteration features Mr. Kazuhiko Maekawa, who had acted as the chairman of HuMA for 10 years until June 2022. Even today, he has involved with HuMA as the adviser while engaging in medical care for the elderly in caregiving facilities. Let’s see what Mr. Maekawa is thinking about at this moment as he has worked on-site at historical accidents and large-scale disasters and moved forward together with the development of Japan’s emergency medical care.
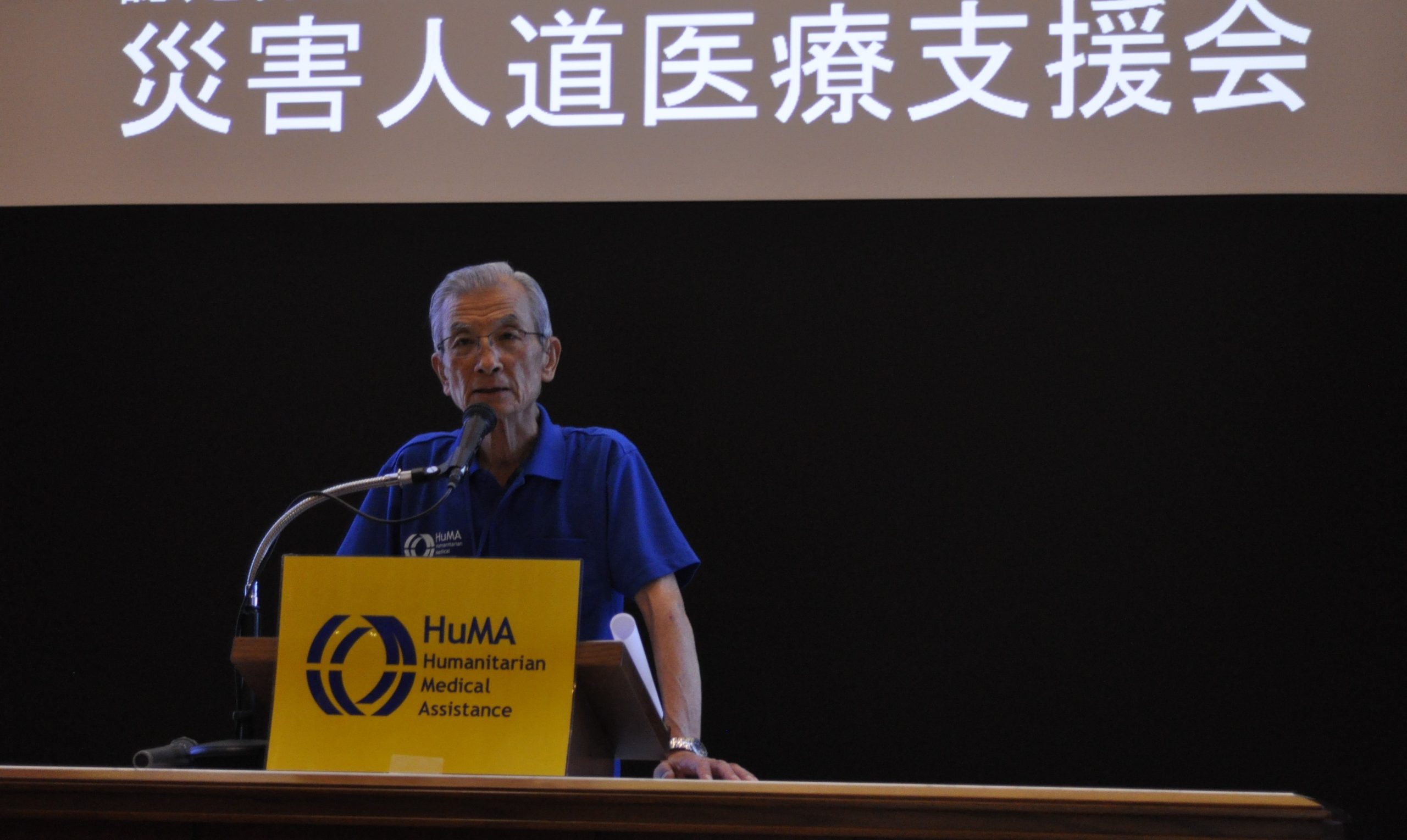 |
| Giving a talk as the chairman during the 2019 Northern Kyushu Heavy Rain Assistance Reporting Session |
World of critical care where immediate decision and teamwork are required
In 1968, I began my career as a surgeon after graduated from university. However, I was increasingly feeling something was missing in my monotonous life since surgical care was provided in a fixed process.
With my feeling, “I want to work at a place where I can feel more changes and dynamism,” I traveled to the U.S and found the world of trauma surgery and seriously ill patient management.
The primary purpose of critical care is literally to save life. We, doctors, are required to make a decision immediately in a situation where there is no time to lose. A slight overlook or slightly late response has a risk of losing a patient’s life. We sometimes confront unprecedented issues. What helps us the most in that situation is teamwork after all.
There was no diagnostic imaging method such as CT or ultrasonography at that time. All the members did our best making excellent use of our knowledge and techniques, so when our medical care worked well, the pleasure was invaluable.
At the sites of the Great Hanshin-Awaji Earthquake, the Tokyo Subway Sarin Gas Attack, the Tokaimura Criticality Accident
After returning from the U.S., I engaged in critical care in Japan and there were three major accidents; the Great Hanshin-Awaji Earthquake in January 1995, the Tokyo Subway Sarin Gas Attack that occurred only two months after the Earthquake, and the Criticality Accident that occurred in a nuclear fuel processing facility in Tokaimura, Ibaraki Prefecture in 1999.
In the Great Hanshin-Awaji Earthquake, a medical team was dispatched from the University of Tokyo Hospital to an evacuation center in Ikuta District, Kobe City. I stayed in Tokyo involving in the assistance activity as a responsible person of the team as it was just after I had undergone gastric cancer surgery. The Earthquake caused profound damage to the area, resulting in the need for not only first aid but also long-term medical care. We also visited there as part of Hyogo Prefecture’s reconstruction verification project five years after the Earthquake to look into the level of reconstruction in the healthcare front.
In the Tokyo Subway Sarin Gas Attack, we provided emergency treatment to those carried to a hospital in Tokyo. The appalling Attack killed 13 people and injured over 5,000 people. This must not happen again but at the same time, this experience of acute care should be conveyed to future generations. We therefore had a questionnaire survey of treatment method for those who was exposed to sarin and hospitalized, and a survey of chronic health damage by sarin.
Thirdly, Tokaimura Criticality Accident. As the unforeseen accident occurred at a place that wasn’t expected from the nuclear fuel cycle, the radiation dose of the on-site workers reached a level that was determined as “unable to survive” given the normal medical standard.
At that time, I was just an acute care physician, not a specialist of treatment for radiation exposure. Nevertheless, someone had to take measures to save their lives even in the face of such a desperate situation.
With that passion in our mind, we made each and every effort as the entire hospital, but unfortunately, two of the victims lost their lives. When I tore off the chest muscle for legal autopsy, the radiation-damaged body made a sound I had never heard. It was at this moment that made me think, “Alas, this is an area beyond the realm of human knowledge” and feel how powerless I was.
Role of the chairman is to back up the assistance activities
In 2011, I assumed the position of HuMA’s chairman after the Great East Japan Earthquake. HuMA mainly consists of volunteer healthcare workers and this aspect sometimes poses challenges such as financial vulnerability and recruitment difficulty. However, I chose to be in charge because I thought my previous experiences would help HuMA on this occasion.
The chairman’s biggest concern is the health and safety of dispatched staff. Particularly if the activity takes place overseas, not only weather and sanitation but also security and political affairs are very different from those of Japan.
In fact, we encountered some dangerous situations: some staff upset their health in the Philippines; the aftershock of a great earthquake occurred in Nepal; the local police temporarily stranded us in Bangladesh.
We cannot provide medical assistance without our health and safety. I always paid attention to the point throughout the on-site activity periods.
As HuMA submits a post-activity report including some advice to sites to which staff were dispatched, the chairman reviews documents compiled by dispatched staff.
A bird does not foul the nest that it is about to leave. One of my important roles was to bring to a close the activities in a way that local people think, “We thank the HuMA team for your coming.”
 |
| In the area hit by a typhoon in Nagano Prefecture in 2019 |
To those who will lead the next generation
I often worked with young staff in disaster-hit areas in Japan. Their energy motivated me through the collaboration and communication between them and me. I think that working on-site in the field of disaster medicine offers those who will lead the future healthcare an opportunity of great importance.
While equipment, material and personnel are often sufficient for medical treatment in hospital in peacetime, you have to perform the best of your potential under restricted conditions in disaster-hit areas.
You spontaneously think and take action to save the life in front of you. I believe that disaster medicine is the starting point of medical ethics.
It is no easy task to seriously engage in a life-saving job, and that is why it is worthwhile doing it.
I sincerely hope that young people with such mind will lead the next-generation healthcare.

(Photo: 2019 HuMA orientation training with an expectation to staff who will lead the next generation.)

